Thank you to WFMZ for including me on a recent episode of Business Matters!

Thank you to WFMZ for including me on a recent episode of Business Matters!


When I’m feeling well, I feel very resilient, but when I’m not—when depression sets in as it inevitably does— I feel weak, like I’ve failed to stay well and I should have known better. I think, “How could I let this happen? Why didn’t I practice my coping skills better? How did I miss the warning signs?” I see others show remarkable resilience through unimaginable losses, severe illnesses, major defeats. I envy them as they bounce back or pivot or at least maintain a positive attitude. I think back to all the struggles and challenges I’d endured before my break—a chaotic childhood filled with divorces, arrests and restraining orders, bankruptcy at 22 due to cosigning with parent, father’s incarceration, three broken engagements, etc. I took it all in stride, barely missing a day of work. I prided myself on my resilience. Nothing seemed to bring me down until a toxic work environment and a cruel supervisor pushed me to the breaking point.
Now I can’t seem to bounce back, pivot, or think positively about anything. What happened to that resilient young woman who took everything in stride? My brain spins in an endless negative loop on a perfectly normal day. It can take the most positive event and turn it into gloom and doom. The slightest thing can set me back and undermine my confidence and worth. It’s like a dam in my brain has broken and it can no longer hold back the flood of negativity. Everyone around me seems to handle life with such grace, productivity, and positivity. I feel weak, lazy, vulnerable, embarrassed, ashamed, scared. I should be more productive, more grateful, more resilient—better.
And yet bipolar disorder is a brain disease. It clouds perceptions and disguises lies as truth. Maybe resilience looks differently for a bipolar person. Maybe resilience is getting up in the morning when a 100 lb weight is holding you down. Or showing up to an event when you want to isolate at home or finishing an assignment when your brain isn’t working. It makes no sense to compare my resilience to someone who doesn’t suffer from a brain disorder. A person with lung cancer will most likely not breathe as well as someone without it. It’s no weakness on that person’s part; it’s the nature of the illness. That person can try and try to breathe better, but it’s not going to happen. They can utilize tools that will help them to breathe easier, but they’re going to struggle to do it on their own. Isn’t the same true for bipolar? I can try and try to stay positive, to not let something get to me, but my brain will go there anyway. The brain can’t think and process things well if it’s sick so I have to use coping skills, medication, therapy to help me breathe easier, too.
It turns out my resilience shows the most when I’m not well. It takes strength to ride out the long and dark days of depression. It takes optimism to maintain a shred of hope when the brain tries to convince you it’s hopeless. It takes persistence to keep going when your body and brain want to give up. Resilience is shown in all kinds of ways and those with mental health conditions model resilience every day of their lives.


Sometimes you can do all the right things (e.g., practice gratitude, mindfulness, reframe distortions, use positive self-talk and affirmations, exercise, eat right) and depression can still rear its ugly old head in and leave you in a world of suck. I’ve really been struggling the past few weeks and my biggest fear is: what if I don’t get better? I know, rationally, that I will get better at some point and I just need to ride out yet another episode, but I still worry that no matter what I do I’ll never get better and I can’t live this way for the rest of my life. I need to remind myself that, as my therapist tells me, “that’s my anxiety and depression talking.” I need to challenge these distortions and tell my depression to “shut up!”
So let me reframe this distortion: “No matter what I do I’ll never get better.” This is not true nor is it helpful. I haven’t tried all possible medications and treatments so I can’t know that nothing will help (generalization). I also can’t know that I will never get better either (mind reading or predicting the future). However, if I tell myself that I won’t get better I will, no doubt, impede my progress.
A more rational thought would be: “There are many medications and treatments I haven’t tried. It may take time, but I will get better as I have many times before.”
Just by reframing my thought, I feel a little better. Each positive step I take is a step closer to wellness. Depression may have me in its grip right now, but I will get better. It’s only a matter of time.

Of all the wellness tips and techniques I’ve learned, the most impactful and surest way for me to stay healthy is through peer advocacy. Sharing my story and providing hope to others gives me purpose and value. It also reminds me how far I’ve come and how important it is to practice all of the strategies that I have learned along the way. After all, I don’t want to be a hypocrite who says one things but does another. So every time I give a presentation, teach a class, or run a support group, I get the chance to check in with myself. Am I practicing what I’m preaching? It’s a built in self-accountability system, for which I’m incredibly grateful. By helping others, I help myself. For me, it’s a no-brainer.
The value of peer advocacy cannot be overstated. I remember sitting in the hospital or various partial programs thinking, “where are all the people who are living well with mental illness?” I wanted to hear from someone who suffered from severe depression, anxiety, bipolar–someone feeling as hopeless as I did–but had come out on the other side and was doing well. I could read and learn all about mental illness and recovery, but until I saw someone on the outside who was managing their illness and leading a life in recovery, I couldn’t believe that it was possible for me, too. Sure, we read about celebrities with mental illness, which is brave and important, but I wasn’t a celebrity and those examples just weren’t relatable to me. I remember thinking, “If this famous person who has tons of money and resources and support can barely survive, what are my chances?” More often than not, their stories depressed me more.
Sadly, it is not easy to find people with mental health issues who are willing to speak out, especially if they are doing well. There is a definite risk involved and it’s foolish to think otherwise. While some employers may treat workers with mental illness fairly and respectfully, many will not. Once I disclosed my mental health condition, I was treated like a liability after 15 years of exemplary evaluations. Every classroom issue was automatically attributed to something I was doing wrong. Eventually, it reached the point where I had to resign to maintain my health and dignity. Despite valiant efforts to end the stigma surrounding mental illness, it remains as strong as ever and it silences peers who could give so much hope to others. I get it, though. I really do. When you work like hell to get yourself employed again, you certainly don’t want to risk your job by revealing a mental health condition. Rather than seeing the ability to manage an illness as a testament to a person’s strength, bravery, and resilience, some will, undoubtedly, view it as a weakness and treat him/her/them as less than.
Through my advocacy, I hope to inspire others to speak out and share their truth. Right now I am the only person who is trained in our NAMI affiliate to teach classes, speak to organizations, and facilitate support groups. There are others who are trained in one or the other, but often it comes down to me. And I can only do so much. We need others and our impact can be great. Until society regularly sees people with mental illness who are skilled, knowledgeable, and successful, the stereotypes and misperceptions will continue. Often the ones who do reveal their mental health conditions have already established themselves as experts or celebrities so they are already acknowledged and accepted in their careers. Of course it helps to hear from those people, but where is the voice of the working class person– the group to which the majority belongs. We are here, but we cannot be heard until more of us speak out and act in ways that dispel all those dangerous misconceptions. If all society sees of mental illness is the lone shooter or a ranting celebrity, how can society change its view on mental health conditions?
Please consider joining me in the fight to give a voice to mental illness–that it isn’t something to fear. It doesn’t just affect that one eccentric relative that others tell funny stories about–or won’t talk about at all. Since one out of four people in the US has a mental illness, chances are you know someone right now who is suffering. It might be the person you least expect, too. Most people with mental health conditions are experts at hiding it, (which is sad since they should be using the little bit of energy they have for self-care). Furthermore, no one is immune. I never thought it could happen to me. Until it did.
It’s time to end the silence that perpetuates the stigma surrounding mental illness. By sharing and listening to each other’s stories, we validate each other and strengthen our collective voice. As peers, we have the power to truly make a difference in the way that no other source can.

So grateful to have been included in the mental health initiative panel discussion with Governor Wolf, Rep. Mike Schlossberg, and Dr. Rachel Levine held today at Muhlenberg College. Through new initiatives and candid conversation, I am hopeful that mental health will receive the same attention, care, and consideration as physical health conditions. By speaking out, eliminating barriers, and improving the quantity and quality of resources, countless lives will be saved and hope and dignity will be restored to those suffering from mental health conditions. Stand proud and speak your truth!
To read more about this event, click here
ON RECOVERY
Recently, a friend shared the following post regarding her recovery from cancer on Facebook:
“I’ve been cancer-free for almost nine months. Some days, I can’t tell if I’m recovering from all of the treatments because it takes so long to recover. But, then I look back on the past nine months and realize that I’ve come a long way. Here’s how I know I’m getting better:
-9 Months Ago: Couldn’t do three push-ups without collapsing.
-Today: Did 20 of them.
-9 Months Ago: I could barely lift 20 pounds.
-Yesterday: I did 48kg deadlifts (I forget how to convert that number into pounds).
-9 Months Ago: Couldn’t run a mile in less than 14 minutes.
-Today: I run multiple miles in less than 12-minute miles… getting closer to 11-minute miles.
-9 Months Ago: Sometimes, I slid down the stairs because chemo made my feet numb and it was easier to slide than try to walk down the stairs.
-Today: I still hold onto the railing for dear life, but I let go on the last few stairs, now.
So, when I type it out like this, I see that there is so much to celebrate on this birthday. I’m still praying for a full recovery, but, really, I’m just grateful to be here and to know so many wonderful people”
***************************************************************************
Naturally, I was thrilled to read of her progress and all the supportive comments that followed her post. Then I thought about how far I’ve come with my own illness and I felt grateful, too. But I wondered: what responses would I get if I posted my progress regarding my mental health condition? Would people think I was just seeking attention, exaggerating, or minimizing my friend’s struggle with cancer? Would others even read it? If they did, would they just roll their eyes and move on? Or would they avoid me the next time they saw me in person, as if my depression might somehow infect them?
I understand that people might not know what to say to someone who struggles from depression, but saying nothing just makes a person feel more ashamed, more worthless, more invisible, and more alone. So here is my celebration of my progress within the past 7 years
My Recovery from a Mental Health Condition:
“7 years ago, my brain broke and I was diagnosed with bipolar II and major depression. I felt like I was given a death sentence, because there is no cure for mental health conditions and I will never be “free” of it. Some days, I struggle with feelings of worthlessness, fatigue, and loss of purpose and identity; It all seems too much to bear. But, then I remember how far I’ve come and how much I’ve learned. Here’s how I know I’m doing better:
-7 Years Ago: I was so ashamed and embarrassed, I isolated. I had no idea what was wrong with me or how to get better.
-Today: I have shared my story publicly and strategies I use to stay well with hundreds of patients and peers and teach NAMI education courses on an ongoing basis.
-7 Years Ago: I had 30 rounds of ECT and had difficulty remembering things and communicating my thoughts.
-Today: I regained my short-term memory, my brain responds to medication, and I am able to manage side effects.
-7 Years Ago: I was unable to work and convinced I’d never work again, let alone teach.
-Today: I have several jobs that allow me to use the skills I’ve spent my whole life building (NCC, NAMI, PBS, and TUTOR DR)
-7 Years Ago: I wanted to die to stop the persistent feelings of worthlessness, hopelessness, and despair
-Today: I enjoy life and I know I have worth, purpose, and hope.
-7 Years Ago, I could barely get out of bed, get dressed, shower, and complete basic household chores
-Today: I get out of bed, complete household chores, and take care of my child on a regular basis.
-7 Years Ago: I didn’t even want to leave the house and took no pleasure in any of the things I once loved.
-Today: I direct school plays, sing in a band, perform in community theatre, and maintain my own blog.
So, when I type it out like this, I see that there is so much to celebrate, though many will still consider me “weak,” “lazy,” “crazy,” or “over-dramatic.” I know this will be a lifelong battle and there will be relapses, but I’m grateful to be here and to have the knowledge and skills to manage my condition, educate the public, and inspire hope to others with mental health conditions.
Why is a mental health condition treated differently than a physical one? Both are life-threatening medical conditions that affect millions of people. Both require extensive treatments and medications with crippling side effects. Yet someone with cancer is accepted, acknowledged, and supported while someone with a mental health condition is questioned, avoided, shamed, and blamed. No one says to someone with cancer, “get over it,” or “you’re just too lazy to work” or “you just want sympathy” or “there are days I feel like I have cancer, too.” That would be ridiculous. Yet, people with mental illness hear that all the time. Is a person who is battling mental health condition any less of a warrior, role model, or hero? My friend is resilient, strong, and courageous. So am I. So is anyone who fights daily to overcome any other debilitating disease. Just because an illness cannot be seen doesn’t mean it isn’t there or is any less serious.
Until mental health conditions are given the same respect, attention, and care as physical health conditions, the stigma surrounding mental illness will continue and people will suffer in silence and shame. Precious lives will be taken that might have been saved. If you are struggling with mental illness, you are not alone. You are seen, heard, honored, and loved more than you could ever know. Fight on, brave warrior—we see you, we hear you, we honor you.
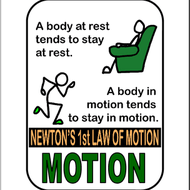
I’m no scientist and I don’t remember much about Physics, but I know all about inertia. It is easy for me to get stuck in a rut and I have to really push myself to get motivated. Some days are easier than others, but one thing’s for sure: lying on my couch doesn’t help. Once I get sucked into the couch vortex, I can disappear for hours. One hour leads to another and another. Before I know it, the day is almost over and I accomplished nothing. Then I think of all the things I should have done. Then I feel the guilt and shame and worthlessness. It’s a vicious cycle–the less I do, the worse I feel, and the more negative my thoughts become. So what does this have to do with Newton’s first Law of Motion? Everything.
In a game of dominoes, the dominoes remain still until one topples. When one moves, it causes the next to fall and so on. Bodies are no different. That’s why I need to make sure I get up and move during the day. It doesn’t need to be exercise or anything in particular, but if I don’t force myself to get up, I can easily stay there for a long time. Then the feeling and thoughts get going and soon I’m spiraling down a dark dark hole. However, if I can take one step no matter how small–topple one domino–it will often lead to the next one and I gain momentum.
The tricky part is that unless I have to be somewhere, I tend to stay put. Then I feel even worse for not doing anything when I had the time and the means. I swear working full-time is what kept me sane all those years. The great irony is that my mental illness prevents me from working full-time: I can’t handle the workload or the level of stress I took on before. It’s a constant challenge, but I try to catch it early and set myself in motion, often through the encouragement or accountability by a friend, peer, family member, therapist, etc. Many have told me that having a pet has saved their lives. Their pets give them purpose and force them to get up and walk them, feed them, play with them, and care for them. My pet, a sweet rescue cat named “Cinnamon,” prefers the couch so he isn’t much help in the get-up and get-moving department. He does give me joy, though. Thankfully, I have other things that keep me moving.
Finding ways to build in accountability and maintain a consistent routine can help so much. For me, volunteering and partial programs gave me that structure when I wasn’t able to provide it on my own. I had a specific time and place I needed to be. My therapy appointments and peer support group meetings helped me to get out, even if just for an hour or two. I learned to be gentle with myself and give myself credit for even the small tasks I completed. It feels good to cross something off a list, no matter how small it is. Accomplishing a goal builds momentum and moves energy in the right direction.
I still find myself drawn to the siren song of the couch, but it’s getting easier to steer away toward brighter shores. Sure, there are days I succumb and and crash, but I give myself grace, get back in my ship, and move on.
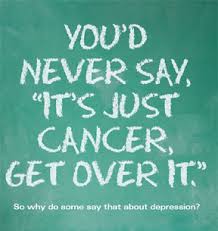
“Get over it.” This is one of the most frustrating responses I get during a bout of depression. Telling someone to “get over it” is like telling someone with broken legs to run a marathon. It defies common sense as depression affects the brain’s ability to think clearly in the first place. Others recommend going for a run or to the gym. If it were that simple, I would have already done that. I know that exercise helps with depression, but when just getting out of bed takes monumental effort, there isn’t much energy left for lacing up.
I don’t blame people who give this advice–in fact, I used to be one of them. I could never have realized the debilitating effects of depression until I experienced them firsthand. However, telling someone who is depressed to just “tough it out” or “snap out of it” points to a profound ignorance about mental health. No one would tell someone with cancer to just “deal with it” (nor should they), but depression is a life-threatening disease as well. Contrary to popular belief, depression is not just feeling tired or sad and upset over a recent loss. It is a serious life-long illness that requires treatment and while it can be managed with medication and lifestyle changes, there is no cure.
Sadly, there are many factors that prevent people from seeking help for a mental health condition. Perhaps the biggest deterrent is the stigma associated with mental illness. It seems mental illness only gets attention when some “crazy” person goes on a shooting rampage or a celebrity suffers a mental breakdown or commits suicide? This type of attention sensationalizes mental illness, instills fear, and attributes it to “the others”–often, the rich and famous or the truly criminal or deranged. It only perpetuates the stereotypes and misconceptions surrounding mental illness. Most mentally ill people do not commit crimes and should not be feared. Furthermore, mental illness affects people of all ages, races, genders, social classes, professions, etc. In fact, the National Institute of Health indicates that mental illness afflicts one in five American adults in any given year, and yet it remains a taboo and often misunderstood subject (2018).
Even though mental illness can be caused by environmental stresses, genetic factors, biochemical imbalances, or a combination, many view those with mental health conditions as “weak” or “lazy” or somehow at fault. Some of my own family members and friends have simply rolled their eyes at my pain and chalked it up to my being “dramatic” or “attention-seeking.” So, not only is someone with mental illness feared, he or she is further burdened with additional labels and made to feel “guilty,” “lazy,” or “ridiculous.” It is no surprise that so many people with mental illness feel rejected or ostracized, which only enhances isolation and feelings of worthlessness. When someone is seriously ill, people often rush to his or her aid delivering meals, sending flowers and cards, visiting them, and/or helping with household tasks or children. Cancer survivors are rightfully referred to as “warriors,” “survivors,” and “heroes.” But even though those with mental illness suffer, fight, and overcome tremendous battles as well, they are seldom honored and celebrated. Many survivors of serious health conditions say they could not have done it without the support of family, friends, colleagues, neighbors, yet many with mental illness find themselves with little support and few allies.
The shame and stigma with mental illness is so prevalent that some would rather suffer in silence (or even end their lives) than admit they have a mental disorder and seek help. Suicide is the 3rd leading cause of death in youths 10-24 and these rates are only rising (NAMI, 2018). Adolescents suffering from clinical depression increased by 37 percent between 2005 and 2014 (John Hopkins Health Review, 2017). Approximately 11 million U.S. adults aged 18 or older had at least one major depressive episode with severe impairment. (NIH, 2017). Clearly these statistics indicate a dire need for mental health intervention, yet there remains a significant deficit in providers and insurance coverage. Mental health programs continue to be cut or insufficiently funded. Research shows that nearly 60% of adults with a mental illness did not receive treatment (NAMI, 2018). With the lack of accessible treatment and the cost of comprehensive mental health care, on top of the stigma, it is not surprising that depression is the leading cause of disability worldwide (World Health Organization, 2017).
With limited access to care, those with mental illness often self-medicate with drugs and alcohol. In fact, 10.2 million adults have co-occuring mental health and addiction disorders (NAMI, 2018). Sadly, drugs and alcohol can be quicker and easier to obtain than an appointment with a therapist or psychiatrist. Furthermore, adding drugs and alcohol to mental illness compounds an already precarious situation. Mental illness can even be triggered by the use of drugs and alcohol. Like most illnesses, early intervention is key and yet little is being done with regards to mental illness other than sensational news coverage and punitive measures. There are valiant community efforts, support groups, dedicated volunteers, and a variety of helpful services and programs, but they are often limited in size and finances.
When will those with mental illness be treated with the dignity they deserve and not forced into silence and shame? When will mental health coverage and the number of providers and services meet the need? There is no simple solution, but each step, no matter how small, makes a difference. Each donation to mental health organizations such as the National Alliance on Mental Illness or the American Foundation for Suicide Prevention (AFSP), each time we speak out for those who cannot or lend a hand or call a friend, we are one step closer to change.
We never know who might be affected. It could be a family member you haven’t heard from in awhile, or a friend who suddenly stops coming to social events or a colleague who is out on a “medical leave.” It might be a child who smiles and seems to have it all, but self-harms behind closed doors. Now is the time to speak out, to share stories, to withhold judgment, to offer support, to seek treatment, to break down the wall of stigma before it takes the life of someone you know and love.